Enquire Now
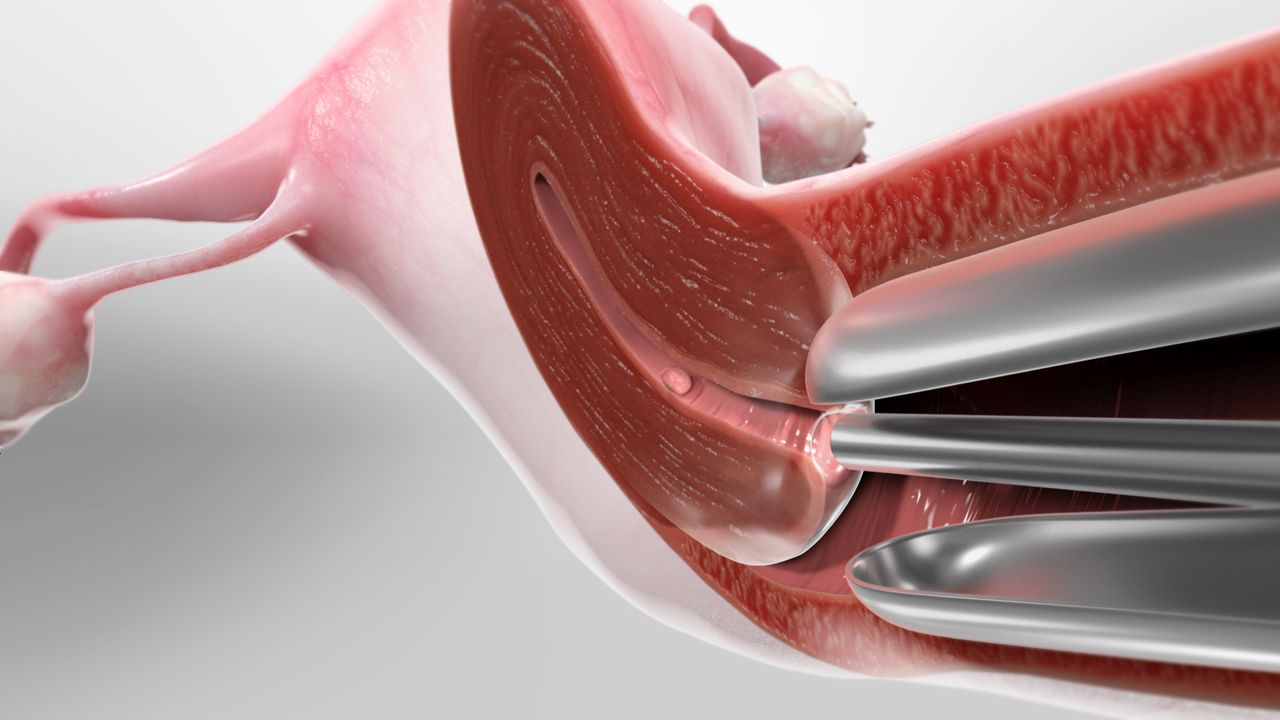
A hysteroscopy is a medical procedure used to examine the inside of the uterus (the womb) and diagnose or treat various gynecological conditions. It involves the use of a hysteroscope, which is a thin, lighte tube with a camera and sometimes surgical instruments attache to it. The hysteroscope is insert through the vagina and cervix and into the uterine cavity to provide a direct view of the uterus. Visit Our Clinic Or more info contact us!
A hysteroscope is a thin, light tube that a surgeon inserts through your vagina to examine your cervix and the inside of your uterus.
Hysteroscopy can be a part of the diagnostic process, as well as the treatment process.
What happens during a hysteroscopy?
Positioning:
- You’ll lie on an examination table, often in the same position as during a pelvic exam, with your feet in stirrups.
Cervical Dilation (If Need):
- In some cases, your healthcare provider may need to dilate (open) your cervix slightly to allow the hysteroscope to pass through. This is done using dilators or medication.
Insertion of the Hysteroscope:
- The healthcare provider gently inserts the hysteroscope through your vagina and cervix and into the uterine cavity. The hysteroscope has a light and a camera at its tip, allowing the provider to view the uterine lining on a monitor.
Visualization:
- As the hysteroscope is advance into the uterus, your healthcare provider will slowly fill the uterine cavity with a sterile fluid (usually a saline solution) to expand it. This helps provide a clearer view of the uterine walls and any abnormalities.
How safe is hysteroscopy?
Type of Hysteroscopy:
- Diagnostic hysteroscopy, which is performe primarily for visualization and evaluation, tends to be less invasive and associate with lower risks compare to operative hysteroscopy, where treatments or interventions are performe.
Anesthesia:
- The type of anesthesia use can influence safety. Local anesthesia or conscious sedation is often use for hysteroscopy, and these are generally safe. General anesthesia carries a slightly higher level of risk but is still consider safe when administer by trained professionals.
Experience of the Healthcare Provider:
- The skill and experience of the healthcare provider performing the hysteroscopy play a crucial role in its safety. An experience provider is better equipp to handle any unexpect complications that may arise during the procedure.
Possible Risks and Complications:
- While uncommon, potential risks and complications associated with hysteroscopy may include infection, bleeding, injury to the uterus or nearby structures, reaction to anesthesia or medications, and complications relate to any treatments performe (e.g., uterine perforation during removal of uterine fibroids).
Patient Factors:
- The patient’s overall health and medical history, including any underlying medical conditions or allergies, can influence the safety of the procedure. Patients with certain medical conditions may have a higher risk of complications.
treatments that infertility specialists
Polypectomy: Thus, Removal of uterine polyps, which are noncancerous growths that can cause irregular bleeding or infertility.
Myomectomy: Once, Removal of submucosal fibroids, which are noncancerous growths in the uterine wall that can lead to heavy menstrual bleeding or fertility problems.
Endometrial Ablation: Therefore, A procedure to destroy or remove the lining of the uterus (endometrium) to treat heavy menstrual bleeding or abnormal uterine bleeding. Firstly, Techniques include thermal ablation, radiofrequency ablation, or laser ablation.
Septoplasty: Thus, Correction of a uterine septum, a congenital condition in which a wall or partition divides the uterus. Once, This can be done to improve fertility or reduce the risk of miscarriage.
Adhesiolysis: Thus, The removal or separation of uterine adhesions or scar tissue. once, which can develop after surgery, infection, or trauma and may cause infertility or menstrual disturbances.
