Enquire Now
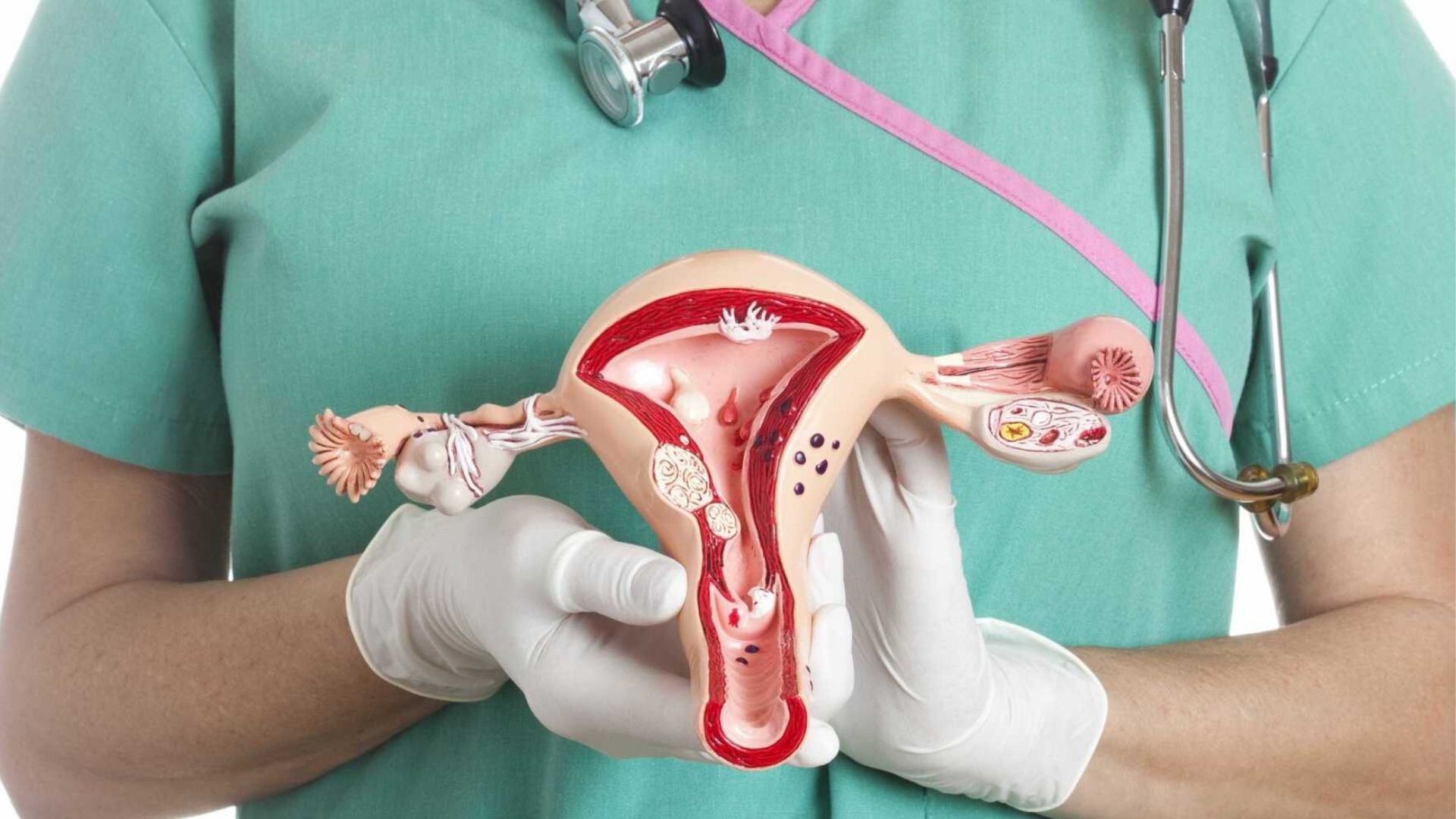
A hysteroscopy is a medical procedure use to examine the inside of the uterus (the womb) and diagnose or treat various gynecological conditions. It involves the use of a hysteroscope, which is a thin, light tube with a camera and sometimes surgical instruments attach to it. The hysteroscope is insert through the vagina and cervix and into the uterine cavity to provide a direct view of the uterus.
Hysteroscopy is a procedure that looks inside of your uterus in order to diagnose. They treat the causes of abnormal bleeding.Visit Our Clinic Or more info contact us!
Hysteroscopies can be perform with local, regional, or general anesthesia, depending on the complexity of the procedure and the patient’s comfort. Some diagnostic hysteroscopies can be done without anesthesia.
responsibilities of a Hysteroscopy
Patient Evaluation: Assessing the patient’s medical history, symptoms, and any relevant diagnostic tests to determine the need for a hysteroscopy.
Inform Consent: Explaining the procedure, its purpose, potential risks and complications, and obtaining the patient’s inform consent before the procedure.
Preparation: Ensuring that the patient is appropriately prepare for the hysteroscopy, which may include instructions about fasting or taking medications before the procedure.
Anesthesia: Deciding on the type of anesthesia (local, regional, or general) and administering it as need to ensure the patient’s comfort during the procedure.
Procedure Execution: Performing the hysteroscopy by inserting a hysteroscope into the patient’s uterus through the vagina and cervix. The healthcare provider may use the hysteroscope for diagnostic purposes or to perform specific treatments, such as polypectomy, myomectomy, or endometrial ablation.
Safety: Ensuring the safety of the patient throughout the procedure, including monitoring vital signs, managing any complications that may arise, and using appropriate sterile techniques.
Treatment Decisions: If the hysteroscopy is for therapeutic purposes, making inform decisions about the appropriate treatment base on the findings during the procedure.
How do I get ready for a hysteroscopy?
Patient Evaluation: Assessing the patient’s medical history, symptoms, and any relevant diagnostic tests to determine the need for a hysteroscopy.
Inform Consent: Explaining the procedure, its purpose, potential risks and complications, and obtaining the patient’s inform consent before the procedure.
Preparation: Ensuring that the patient is appropriately prepare for the hysteroscopy, which may include instructions about fasting or taking medications before the procedure.
Anesthesia: Deciding on the type of anesthesia (local, regional, or general) and administering it as need to ensure the patient’s comfort during the procedure.
Procedure Execution: Performing the hysteroscopy by inserting a hysteroscope into the patient’s uterus through the vagina and cervix. The healthcare provider may use the hysteroscope for diagnostic purposes or to perform specific treatments, such as polypectomy, myomectomy, or endometrial ablation.
Safety: Ensuring the safety of the patient throughout the procedure, including monitoring vital signs, managing any complications that may arise, and using appropriate sterile techniques.
Treatment Decisions: If the hysteroscopy is for therapeutic purposes, making inform decisions about the appropriate treatment base on the findings during the procedure.
Documentation: Recording details of the procedure, including any findings, treatments perform, and any complications encounter.
Post-procedure Care: Providing post-procedure care instructions to the patient, including information on what to expect in terms of recovery, potential side effects, and when to seek medical attention if necessary.
Risk Factor
Hysteroscopy is consider a safe procedure with low risk. However, like any medical procedure, there are potential risks, which may include infection, bleeding, injury to the uterus or other nearby structures, and adverse reactions to anesthesia or medications.
